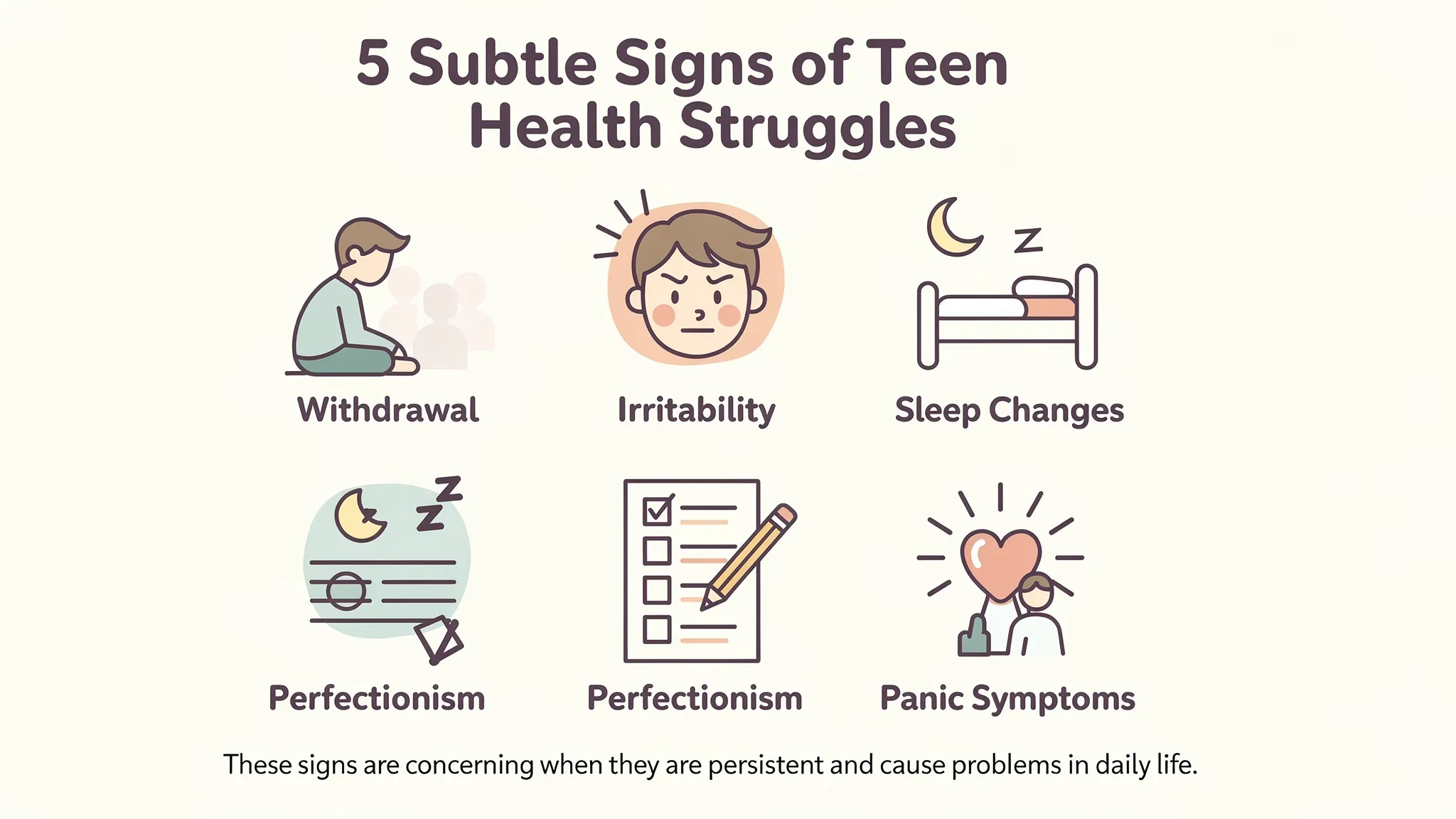
Teen anxiety and depression rarely look like the dramatic “crying every day” stereotype. In NYC especially, many teens learn to mask what they feel with a convincing “I’m fine,” then keep going through school, sports, and social commitments on sheer adrenaline. What parents tend to notice first is not sadness, it’s a quieter shift: more irritability, more shutdowns, more sleep issues, more perfectionism, and fewer real moments of ease.
If you are wondering whether your teen needs a teen anxiety psychiatrist in NYC, if you’re looking for specialized support, Dr. Yana Serobyan, MD, DO (board-certified child & adolescent psychiatrist), works with NYC teens experiencing anxiety, depression, panic, and school stress. It’s to recognize patterns early and get the right level of support before symptoms harden into avoidance, school refusal, panic, or a depressive spiral.
Why teen anxiety and depression can be hard to spot
Adolescence is a developmental period in which privacy, independence, and emotional intensity increase simultaneously. Add NYC stressors (competitive schools, long commutes, packed schedules, social media pressure, and limited downtime), and many teens present with “functional distress”: they still perform, but it costs them.
A few reasons symptoms stay hidden:
- Irritability can replace sadness. Depression in teens often shows up as anger, sensitivity, or constant “annoyed” energy.
- Avoidance is easier to see than fear. Anxiety may look like procrastination, excuses, or “forgetting,” not worry.
- Sleep changes blur everything. Poor sleep can mimic or worsen both anxiety and depression.
- Perfectionism can be praised. A teen who is anxious may look like a high achiever until they crash.
- Masking is common. Many teens save their distress for late-night hours, group chats, or private scrolling.
Subtle signs NYC parents often miss, and what they can mean?
No single sign “proves” anxiety or depression. What matters is duration, intensity, and impairment (how much it interferes with school, relationships, health, or daily functioning).
Withdrawal that looks like “normal teen independence.”
Some independence is normal. But concerning withdrawal is more like a shrinking life:
- Quitting clubs, sports, or friend groups without replacing them
- Spending most non-school time alone, often behind a closed door
- Avoiding family meals or becoming unreachable
- Losing interest in things they used to care about
Withdrawal can be linked to depression, social anxiety, panic symptoms, bullying, trauma, or even burnout.
Irritability, explosive reactions, or a “short fuse.”
A teen who is anxious or depressed may feel constantly overstimulated. Small requests can trigger big reactions because their nervous system is already running hot.
Look for patterns like:
- Frequent arguments that start from minor issues
- Rigid “no” responses and difficulty transitioning
- Tearfulness or anger after school (when they finally exhale)
Irritability is not “just attitude” when it’s persistent and accompanied by sleep changes, avoidance, or a decline in mood.
Sleep changes, not just staying up late.
Sleep is one of the most sensitive indicators of mental health in adolescents.
Common red flags include:
- Insomnia (trouble falling asleep, staying asleep, or early morning waking)
- Revenge bedtime procrastination (staying up late to reclaim control)
- Hypersomnia (sleeping excessively, still exhausted)
- Daytime sleepiness affects school performance
Chronic sleep disruption can worsen anxiety and depression, and it can also make ADHD symptoms more noticeable.
For more context on how sleep interacts with mental health, the American Academy of Sleep Medicine and the CDC’s sleep resources offer helpful overviews.
Perfectionism, overchecking, and fear of making mistakes
Perfectionism is often anxiety in a socially acceptable disguise.
Examples:
- Rewriting assignments repeatedly, spending hours to get “exactly right.”
- Melting down over a B, or refusing to submit work unless it feels perfect
- Needing constant reassurance (“Is this okay?” “Did I mess up?”)
- Avoiding new activities unless they can be “the best” immediately
In NYC, this can be amplified by school culture and competitive peer environments.
Physical symptoms that keep recurring
Teens often somatize emotional distress. If your teen frequently complains of physical symptoms, consider whether anxiety could be contributing, especially when medical workups are normal.
Common anxiety-related physical symptoms include:
- Stomachaches, nausea
- Headaches
- Tight chest, shortness of breath
- Dizziness
- Racing heart
Panic symptoms sometimes mistaken for asthma or “random episodes”
Panic attacks can feel like a medical emergency, and teens often fear they are “going crazy” or dying.
If your teen is having sudden waves of intense fear with physical symptoms, this can be panic. Learning the difference between a one-off panic attack and panic disorder can guide treatment. Your family may find this explanation helpful: Panic Attacks vs. Panic Disorder.
“I’m fine” masking and emotional numbing
Some teens do not look sad. They look flat, detached, or “checked out.”
Watch for:
- Very short answers, minimal emotional range
- Going through the motions without enjoyment
- A sense that nothing matters, or everything feels pointless
Masking is especially common in teens who feel pressure to seem “strong,” high-performing, or low-maintenance.
Appetite and energy shifts
Changes can go either direction:
- Eating far less or far more
- Weight changes (up or down)
- Low energy, slowed movement, “heavy” mornings
Changes in appetite can also be related to disordered eating, which requires specialized evaluation.
A quiet drop in grades, organization, or attendance
Academic changes can reflect many issues (learning differences, ADHD, stress, depression, anxiety). The key clue is the change from baseline.
If your teen suddenly cannot initiate work, can’t focus, or starts missing school, an evaluation can clarify whether anxiety, depression, ADHD, or a combination is driving the change.
Self-harm, substance use, or risky behavior
These are not “attention-seeking.” They are often attempts to regulate overwhelming emotions, numb distress, or fit in socially.
If you notice self-harm marks, vaping escalation, binge drinking, or dangerous impulsivity, it’s a sign to get professional support promptly.
Quick comparison: anxiety vs. depression and overlap.
Anxiety and depression frequently co-occur in adolescents, and symptoms can blend.
| Pattern you see at home | Anxiety often sounds/looks like | Depression often sounds/looks like |
|---|---|---|
| Avoidance | “I can’t do it,” procrastination, excuses | “What’s the point?” withdrawal, giving up |
| Mood | Tense, irritable, keyed up | Flat, irritable, hopeless, easily frustrated |
| Thoughts | Worry, catastrophizing, and perfectionism | Self-criticism, worthlessness, guilt |
| Body | Restlessness, stomachaches, panic symptoms | Fatigue, low motivation, sleep/appetite changes |
| School | Overworking, overchecking, fear of mistakes | Missing work, low drive, slowed performance |
If ADHD is in the picture, it can complicate everything. Executive function struggles can trigger anxiety (“I’m always behind”), and chronic negative feedback can contribute to depression.
When symptoms are urgent, and when to seek emergency help?
If your teen expresses suicidal thoughts, talks about wanting to die, has a plan, is self-harming with medical risk, or you feel you cannot keep them safe, seek immediate help.
In the US:
- Call or text 988 (Suicide and Crisis Lifeline): 988lifeline.org
- In NYC, you can also contact NYC Well: nycwell.cityofnewyork.us
- If there is imminent danger, call 911 or go to the nearest emergency room
Even if you are unsure, it is appropriate to consult a professional urgently.
To help you gauge severity, here is a practical reference table.
| Sign | Consider it more serious when… | What to do next |
|---|---|---|
| Withdrawal | They stop seeing friends, stop activities, avoid family consistently | Schedule an evaluation, ask school counselor for input |
| Irritability | It’s daily, escalating, or paired with hopeless talk | Seek clinical assessment, consider therapy and family support |
| Sleep disruption | It lasts weeks and impairs school or mood | Prioritize sleep assessment, consider CBT-I strategies |
| Panic symptoms | They avoid places due to fear of attacks | CBT targeting panic, consider medication evaluation |
| Self-harm / suicidal talk | Any mention of wanting to die, planning, or escalating self-harm | Urgent crisis support, same-day evaluation if possible |
What actually helps: evidence-based supports for teens
The best plan depends on your teen’s symptoms, medical history, family context, and whether there are learning or attention concerns. In general, these approaches have strong evidence in adolescent anxiety and depression.
1) A thorough evaluation before you assume it’s “just stress”
A good adolescent mental health evaluation typically includes:
- A teen interview (private time with the clinician is important)
- Parent input and developmental history
- Symptom screening tools for anxiety and depression
- Safety assessment (including self-harm and suicidal ideation)
- Review of sleep, substances, medical issues, and medications
- School input when relevant
When attention, learning, or cognitive concerns are present, formal testing can be useful to clarify ADHD, learning differences, or cognitive patterns that may be feeding anxiety or depression.
2) Therapy that fits the problem and the teen
For many teens, therapy is the core treatment.
- CBT (Cognitive Behavioral Therapy) is a first-line treatment for many anxiety disorders and depression, teaching teens to identify thought patterns, build coping skills, and gradually face avoided situations.
- DBT (Dialectical Behavior Therapy) skills can be particularly helpful for emotion regulation, distress tolerance, and self-harm risk.
- Supportive therapy can help teens process stressors, build insight, and feel less alone, especially when symptoms are milder or therapy is a first step.
The best therapy is the one your teen can engage with consistently.
3) Teen therapy and medication when appropriate
For moderate to severe anxiety or depression, combining therapy with medication can be effective. Medication decisions should be individualized and carefully monitored, especially in adolescents.
Common medication classes used in adolescent anxiety and depression include SSRIs (selective serotonin reuptake inhibitors). These medications have FDA boxed warnings about increased risk of suicidal thoughts/behavior in children, adolescents, and young adults, particularly early in treatment, which is why careful follow-up and family monitoring are essential. You can read the FDA’s overview here: FDA antidepressant use in children and adolescents.
Medication is not “a personality change.” When it works well, families often describe the teen as more like themselves: less stuck, less flooded, more able to use therapy skills.
4) School coordination and NYC-specific pressure points
NYC parents often feel trapped between “push them to keep up” and “pull them back to protect them.” A clinician can help you find the middle path.
Supports can include:
- Coordinating with school counseling teams
- Academic accommodations (when clinically appropriate)
- Planning gradual re-entry if avoidance or school refusal is developing
If anxiety signs are showing up in a younger child as well, this post can help you compare what’s developmentally typical vs concerning: Childhood Anxiety Red Flags Every NYC Parent Should Know.
5) Lifestyle supports that are not “just self-care.”
Lifestyle changes are not a substitute for care when symptoms are significant, but they do matter.
Focus on:
- Sleep consistency same wake time, wind-down routine, reduce late-night scrolling
- Movement most days even walking
- Caffeine and energy drinks often overlooked contributors to anxiety
- Structured downtime real recovery time, not just isolated screen time
What to say, and not say, when your teen is struggling
Many NYC parents are problem-solvers. Teens in distress often need validation before solutions.
Try language like:
- “I’ve noticed you seem more on edge, and you’re sleeping less. I’m not mad, I’m concerned.”
- “You don’t have to convince me you’re fine. I want to understand what it’s like for you.”
- “Would you be open to talking to someone who helps teens with stress and mood? We can try a few sessions and reassess.”
Avoid:
- “You have nothing to be anxious about.”
- “Just relax.”
- “Other kids have it worse.”
If your teen refuses help, you can still start by speaking with a clinician yourself. Parents often benefit from coaching on how to approach care without escalating conflict.
When to consider an adolescent psychiatrist near Grand Central, and what to expect.
If you are seeing persistent impairment, worsening mood, panic symptoms, self-harm risk, or you suspect your teen may need medication in addition to therapy, it may be time to consult an adolescent psychiatrist.
Families often seek an adolescent psychiatrist near Grand Central (Midtown Manhattan) because it can make appointments easier to fit around school, commuting, and work schedules.
A psychiatry-led plan can be especially helpful when:
- Therapy alone is not moving the symptoms enough
- Symptoms are moderate to severe
- There is a family history of mood disorders
- There are diagnostic questions (anxiety vs depression vs ADHD)
- Sleep disruption or panic is prominent
If you are looking for specialized care, you can learn more about the practice’s child and adolescent psychiatry services and how a multidisciplinary team approach can support both teens and parents.
Telepsychiatry in New York: help that fits real NYC schedules
NYC families often delay care due to logistical constraints: school hours, after-school commitments, parents’ work schedules, or simply the difficulty of crossing the city.
For many teens, telehealth also reduces barriers like:
- Anxiety about going to an office
- Missing class for appointments
- Scheduling across co-parenting arrangements
If your teen is open to virtual care, explore our practice’s telepsychiatry options in New York.
A practical next step plan for parents, without overreacting
You do not need to wait until things are extreme. Early support can prevent months of escalating avoidance and suffering.
A balanced plan usually looks like this:
- Track changes for 2 to 3 weeks (sleep, mood, avoidance, appetite, school stress, panic symptoms)
- Choose one calm moment to talk (not during a conflict)
- Loop in the school if attendance, grades, or avoidance are shifting
- Schedule a clinical evaluation if symptoms persist, intensify, or impair functioning
If you are currently trying to decide whether what you see is “normal stress” or something more, the safest rule is this: if it’s changing your teen’s life, it deserves professional attention.
Getting the right kind of teen depression help in NYC
The goal is not to label your teen. It’s to reduce suffering, restore functioning, and build skills that protect them in the long term.
If you suspect anxiety, depression, panic, or overlapping attention issues, Comprehensive Psychiatric Services in NYC offers evaluation and ongoing care that can include psychotherapy and medication management when appropriate.
You can start by reading the practice’s guide to anxiety warning signs in kids and preteens: Childhood Anxiety Red Flags Every NYC Parent Should Know, then explore child and adolescent psychiatry services or telepsychiatry in New York to find a path that fits your family.