The First Alarm: A Story Many Patients Know
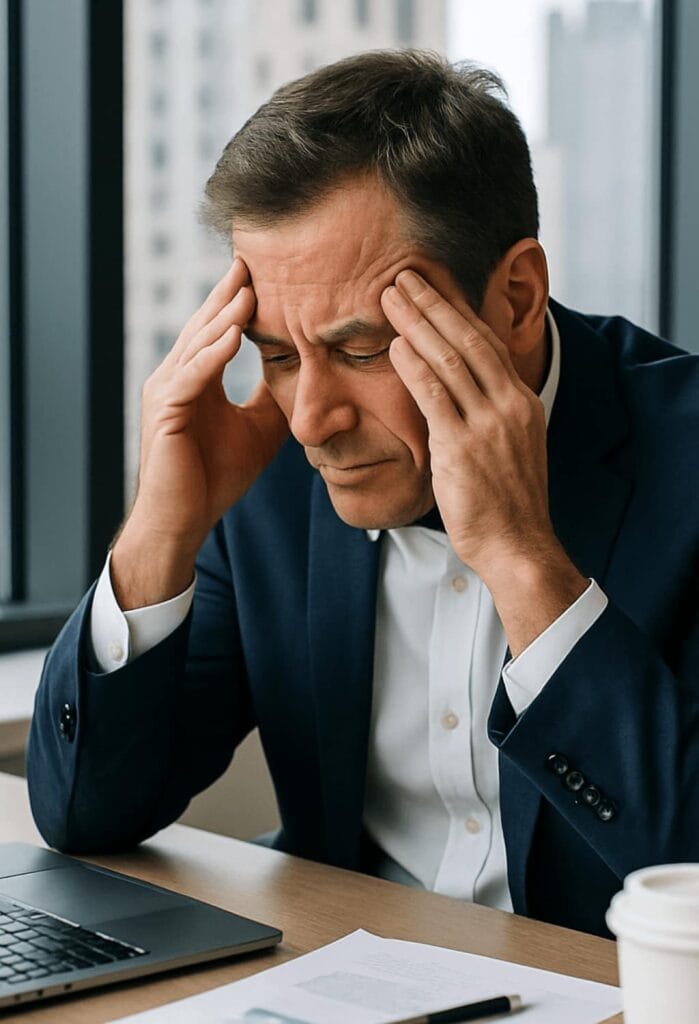
Panic attacks vs Panic disorder. Imagine this: you’re a Midtown Manhattan executive rushing between meetings. Your phone buzzes, emails pile up, and the stress feels manageable until suddenly it isn’t. Out of nowhere, your chest tightens, your heart begins pounding, and your breath feels trapped in your throat. A wave of dizziness makes the room spin, and you’re convinced this must be a heart attack. Your colleagues call 911, but by the time paramedics arrive, the episode has faded. The EKG is normal. The doctor says you’re fine. You leave shaken, but without answers.
That experience was a panic attack—intense, unforgettable, and frightening, yet not life-threatening. For some people, it’s a one-time event, triggered by exhaustion, stress, or even too much caffeine. For others, these attacks begin to repeat. They strike in boardrooms, on subways, in classrooms, or at home. When fear of the next attack begins to dictate daily life, we move from an isolated event into something far more disruptive: panic disorder..
Panic Attacks: The Body’s False Alarm
A panic attack is the body’s alarm system firing when there is no real danger. Think of it as a fire alarm blaring in your office building even though there’s no smoke, no flames, and no reason to evacuate. The system is real, the siren is loud, and your body responds as if there is a crisis. But in reality, nothing is burning.
During a panic attack, adrenaline floods the body. Your heart races, your palms sweat, your breath quickens. Many people describe feeling as if they are choking or being smothered. Others experience chest pain so sharp they are sure it must be cardiac. Some feel dizzy, detached from their surroundings, or convinced they are “going crazy” or about to die. These episodes usually peak within ten minutes, though the aftershocks—exhaustion, fear, unease—can linger much longer.
It’s important to emphasize that while terrifying, a single panic attack is not a psychiatric disorder. Many people will experience one at some point in their lives, particularly under stress. It becomes more concerning when the attacks are recurrent and unpredictable. That’s when we begin to talk about panic disorder.
Panic Disorder: When Fear Becomes the Default Setting
Now consider another story. A college student in New York has her first panic attack underground on a crowded subway. She barely makes it out before collapsing onto a bench, convinced she is suffocating. The attack passes, but the next morning she avoids the subway. Soon she begins skipping classes, terrified of another episode in public. Her world slowly contracts around the fear of panic itself.
This is panic disorder: a condition defined not just by repeated panic attacks, but by the constant anticipation of them. According to the DSM-5, panic disorder is diagnosed when a person experiences recurrent, unexpected attacks followed by at least a month of persistent concern about future episodes or significant changes in behavior to avoid them. In other words, it’s not just the attacks—it’s the shadow they cast over daily life.
When untreated, panic disorder can shrink a person’s world. Students stop attending lectures. Professionals decline promotions or avoid travel. Women navigating life changes—such as menopause, caregiving, or retirement planning—may chalk symptoms up to aging or heart issues, delaying proper treatment. What begins as a misfiring alarm system becomes a constant, exhausting vigilance against the possibility of panic.
Why It Matters for Professionals and Students.
Panic disorder tends to appear in populations that are otherwise high-functioning, which makes it easy to dismiss or hide. Professionals in Manhattan may attribute episodes to long hours, caffeine, or “stress,” while quietly avoiding situations that trigger anxiety. Students often feel embarrassed, assuming they’re weak or failing at independence. “College is supposed to be a fresh start, right …?” Women over 50 may believe their symptoms are tied to menopause or health concerns, not realizing panic could be the true culprit.
In all these cases, the impact is real: careers stall, education suffers, relationships strain, and quality of life erodes. The tragedy is that panic disorder is highly treatable, yet many suffer silently because they either minimize the problem or fear stigma in seeking psychiatric help.

The Hidden Costs of Ignoring Panic
When panic disorder goes untreated, the costs add up quickly. Medical expenses climb from repeated ER visits and unnecessary cardiac tests. Opportunities slip away as patients decline promotions, refuse travel, or withdraw from leadership roles. Relationships strain under the weight of avoidance behaviors loved ones don’t understand. Most painfully, life begins to feel small and constricted. Activities once enjoyed—attending concerts, riding the subway, hosting family dinners—become landmines of potential panic.
Treatment: Evidence-Based, Personalized, and Effective
The good news is that panic disorder is among the most treatable conditions in psychiatry. At Dr. Iospa Psychiatry Consulting Group in Midtown Manhattan, we see executives, students, and women in their 50s reclaim their lives every day.
Treatment often begins with Cognitive Behavioral Therapy (CBT), a gold-standard approach that helps patients retrain thought patterns and break the cycle of fear. CBT teaches practical strategies to de-escalate panic in the moment, while gradually reducing avoidance behaviors.
Medication management is another powerful tool. Selective serotonin reuptake inhibitors (SSRIs) and other evidence-based options can stabilize brain chemistry, reducing both the frequency and severity of attacks. Short-term medication may also be used in the acute phase to provide relief while long-term treatment takes effect.
What sets our practice apart is the integrated model. Our psychiatrists, psychologists, and neuropsychologists collaborate to create personalized care plans. For professionals, this may mean discreet and flexible scheduling. For students, coordination with schools and families. For women in midlife, careful attention to hormonal, medical, and lifestyle factors is necessary. Our goal is always the same: restoring confidence, independence, and calm.
A Patient Story: From Avoidance to Empowerment
One of our patients, a successful Manhattan attorney, avoided the subway for years after a single panic attack underground. She told herself taxis were simply more convenient, but in truth, fear dictated her choices. With careful medication management and CBT, she began gradual exposure therapy—first standing near subway entrances, then taking one stop, and eventually riding again daily. Today she commutes without hesitation, her life no longer run by panic.
Stories like hers remind us that recovery is not only possible, but common. With the right treatment, panic disorder can shift from a life-limiting condition to a manageable challenge.
The Difference That Matters
If you’ve had a panic attack, it doesn’t automatically mean panic disorder. But if the fear of another episode has started shaping where you go, what you do, or how you live, that’s when it’s time to seek professional help.
Panic attacks are isolated events—frightening but short-lived. Panic disorder is the cycle of recurrence, anticipation, and avoidance that can quietly take over a life. The good news is that panic disorder is highly treatable, and recovery is common with the right care.
At Dr. Iospa Psychiatry Consulting Group in Midtown Manhattan, we specialize in helping professionals, students, and women 50+ regain calm and control. Our integrated team of psychiatrists, psychologists, and neuropsychologists works together to reset the body’s alarm system so it rings only when it should.
In the city that never sleeps, where every opportunity counts, don’t let panic define your choices. With evidence-based treatment, you can move past fear and step back into life—confident, focused, and free.