Depression Treatment in Midtown NYC — Recognizing Hidden Signs and Finding Help
Learn how to recognize the subtle symptoms of depression and explore compassionate, evidence-based treatment at Dr. Iospa Psychiatry Consulting Group in Midtown NYC. Our psychiatrists, psychologists, and neuropsychologists hold academic positions at leading New York institutions, including NYU, Mount Sinai, Columbia, and Long Island Jewish Medical Center.
When Stress Feels Like Something More
Living and working in Midtown Manhattan often means running on adrenaline. Many people come to our office saying things like, “I’m just tired,” or “I think I’m burned out.” They assume that exhaustion and emotional flatness are simply part of city life.
But when fatigue, disconnection, or irritability don’t lift with rest, it might be more than burnout. Depression can develop gradually, often blending in with daily stress until it starts to affect every part of life — work, relationships, sleep, and even physical health.
Recognizing that shift is the first step toward getting the right help. Burnout usually improves when you rest. Depression doesn’t. It lingers quietly, even when the pace slows down.
Our Team and Approach
At Dr. Iospa Psychiatry Consulting Group, we believe effective care comes from both knowledge and understanding. Our team includes psychiatrists, psychologists, and neuropsychologists who have trained and taught at some of New York’s leading hospitals.
Several of our clinicians hold academic positions at institutions such as the NYU Grossman School of Medicine, Icahn School of Medicine at Mount Sinai, Columbia University Irving Medical Center, and Long Island Jewish Medical Center (Donald and Barbara Zucker School of Medicine).
These roles keep us connected to the latest research and treatment standards in psychiatry and psychology while allowing us to bring that knowledge directly into our patient care.
Every person’s experience of depression is unique. Our goal is to create a space where patients feel heard and supported, and where treatment plans reflect both science and compassion.
Understanding Depression
Depression is not just “feeling sad.” It’s a medical condition that can look very different from person to person. Understanding the different types helps guide the most effective treatment.
Major Depressive Disorder (MDD)
The most common form of depression. It involves a lasting loss of interest, persistent sadness, and difficulty functioning for at least two weeks or more.
Persistent Depressive Disorder (PDD)
A milder but long-term form of depression that can last for years. Many describe it as “living life on autopilot” — functioning but without joy or motivation.
Seasonal Affective Disorder (SAD)
This form of depression tends to appear in the darker months of the year and often improves with light therapy, psychotherapy, or both.
Perinatal and Postpartum Depression
Depression that develops during pregnancy or after childbirth. It’s more intense than the typical “baby blues” and can deeply affect emotional health and bonding.
Premenstrual Dysphoric Disorder (PMDD)
A severe type of premenstrual syndrome that involves mood swings, irritability, and sadness before menstruation.
Each type of depression has its own characteristics, but all can be effectively treated with the right combination of therapy, medication, and support.

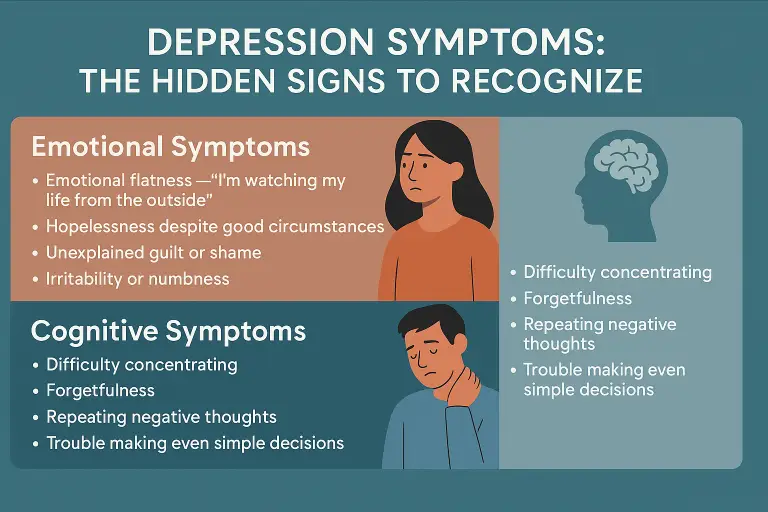
Emotional Signs — When You Feel Disconnected
Depression often doesn’t show up as constant sadness. It can feel more like emotional emptiness — being present but detached.
Common emotional symptoms include:
A sense of emotional flatness, as if watching life from the outside
Hopelessness even when things seem objectively fine
Persistent guilt or shame without clear reason
Irritability or emotional fatigue
One patient once described it as “the lights are on, but I’m not home.” These feelings can be subtle but are often early indicators that something deeper is going on.
Cognitive Symptoms — When Thinking Becomes Difficult
Depression affects concentration and mental clarity. People often find themselves rereading the same page or struggling to make simple decisions.
You might notice:
Forgetfulness or trouble focusing
Slower thinking
Repeating negative thoughts
Difficulty making everyday choices
These cognitive changes are part of how depression impacts brain chemistry and function. They’re not signs of weakness, and they can improve significantly with treatment.

Physical Symptoms — How the Body Reflects the Mind
Depression often shows up in the body before the mind catches on. Many people first visit their primary doctor for physical complaints like fatigue, body aches, or stomach discomfort — only to discover that depression is the underlying cause.
Physical signs can include:
Persistent tiredness or lack of energy
Headaches, muscle pain, or digestive issues
Changes in appetite or weight
Trouble falling asleep or waking too early
Physical Symptoms — How the Body Reflects the Mind
Depression often shows up in the body before the mind catches on. Many people first visit their primary doctor for physical complaints like fatigue, body aches, or stomach discomfort — only to discover that depression is the underlying cause.
Physical signs can include:
Persistent tiredness or lack of energy
Headaches, muscle pain, or digestive issues
Changes in appetite or weight
Trouble falling asleep or waking too early
It’s important to know that these symptoms are real. Treating depression often relieves both emotional and physical discomfort.
Behavioral Changes — Subtle Shifts Over Time
Depression can slowly alter daily routines. People may start skipping social events, letting go of self-care habits, or missing work deadlines. Over time, these small shifts can build into isolation and disconnection.
If you notice that you’re pulling away from friends, avoiding meals, or ignoring texts, it might be a sign that depression is quietly taking hold.
How Depression Looks Different in Everyone
Depression doesn’t have one face. It can look very different depending on your life circumstances and coping style.
Men may express it through anger, irritability, or overworking.
Women might feel anxiety, fatigue, or mood changes around hormonal shifts.
Teens may withdraw, show frustration, or struggle in school.
High-functioning professionals often call it “stress,” even when it’s depression.
No matter how it shows up, depression deserves attention and care — not judgment.
Suicidal Thoughts — A Symptom That Needs Immediate Care
Some people with depression experience thoughts like, “I can’t go on,” or “People would be better off without me.” These thoughts can be frightening, but they are symptoms of an illness — not reflections of truth.
If you or someone you know is in crisis, call or text 988 to reach the Suicide and Crisis Lifeline, or go to your nearest emergency department. Help is available 24/7, and recovery is possible.
For more resources, visit the National Institute of Mental Health’s Suicide Prevention page.
When to Seek Help
If symptoms of sadness, fatigue, or disconnection last for more than two weeks or start interfering with work or relationships, it’s time to seek professional help.
At Dr. Iospa Psychiatry Consulting Group, we offer:
Psychotherapy, including Cognitive Behavioral Therapy (CBT) and other evidence-based approaches
Medication management when needed, using thoughtful and safe prescribing
Neuropsychological testing to evaluate memory and concentration
Collaboration with other healthcare providers for integrated care
Both in-person and secure telehealth appointments
Our goal is to help patients find relief and restore balance in their lives through compassionate, personalized treatment.
Start Your Recovery Today
take the first step
Depression is treatable. Most patients improve with the right combination of therapy, medication, and support. You don’t have to wait until things get worse.
Contact UsFrequently Asked Questions
How do I know if I’m depressed or just burned out?
Burnout typically improves with rest, while depression persists and often affects your energy, motivation, and sense of purpose.
Do you offer online sessions?
Yes. We provide secure telepsychiatry and teletherapy for patients who prefer or need remote care.
Is medication always necessary?
Not always. Many people benefit from therapy alone, while others find that medication management combined with therapy offers the best results.
How soon will I start to feel better?
Most patients begin to notice positive changes within a few weeks of consistent treatment, though recovery is gradual and unique to each person.
Are your clinicians affiliated with major hospitals?
Yes. Several members of our team hold academic positions at leading New York institutions, ensuring that the latest medical understanding informs our care.
About Dr. Iospa Psychiatry Consulting Group
Dr. Iospa Psychiatry Consulting Group is based in Midtown Manhattan and led by Dr. Alla Iospa, a board-certified psychiatrist with extensive clinical experience in mood and anxiety disorders.
Our clinicians also hold academic positions at some of New York’s leading hospitals, including Mount Sinai, NYU, Columbia, and Long Island Jewish. This connection to the academic world allows us to stay current with the most effective, research-based treatments while maintaining a grounded, patient-first approach to care.
We’re here to listen, understand, and guide each person toward lasting emotional wellness.