Sleep, Depression, Anxiety, and PTSD: Unlocking the Brain’s Healing Potential

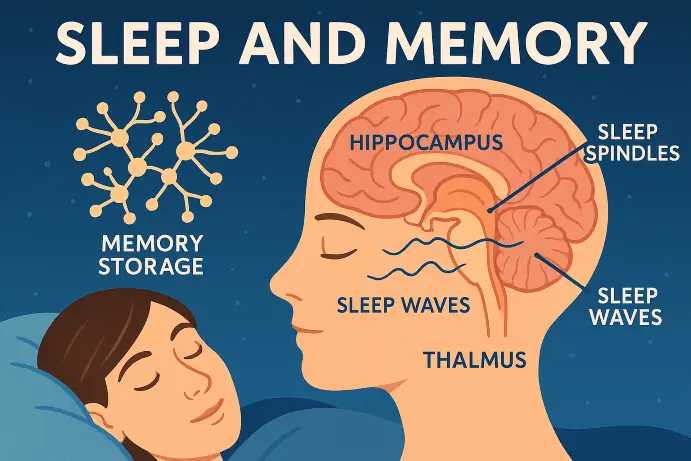
At Dr. Iospa Psychiatry Consulting, we recognize the profound impact of sleep on mental health. For patients struggling with depression, anxiety, and post-traumatic stress disorder (PTSD), restful sleep is often elusive, and its absence can feel like an invisible barrier to healing. But new research is showing that sleep may be more than just a side effect of these conditions. It could be part of the solution.
It’s well known that insomnia and poor sleep quality often accompany psychiatric conditions. What’s less known is that disrupted sleep can actively worsen symptoms, intensifying mood swings, increasing pain sensitivity, and making anxiety harder to manage.
“When sleep falls apart,” explains Dr. William Lu, neuropsychologist and rehabilitation specialist, “everything else starts to unravel too.” In our clinical experience at Dr. Iospa Psychiatry Consulting, this rings especially true for individuals recovering from brain injuries and for those dealing with long-term emotional dysregulation.
CBT-I: A Science-Based Sleep Therapy
One of the most effective, non-medication approaches to treating chronic insomnia is Cognitive Behavioral Therapy for Insomnia (CBT-I). This short-term, evidence-based therapy targets the thoughts and behaviors that interfere with sleep, helping the brain return to a natural sleep pattern.
CBT-I focuses on:
Regulating sleep schedules and habits
Identifying hidden sleep disruptors (like naps or screen time)
Managing nighttime anxiety and racing thoughts
Rebuilding confidence in your body’s ability to sleep
Even more remarkable? CBT-I has been shown to reduce depression and anxiety symptoms, improve energy, and lessen physical pain, without increasing sleep medications.
Treating the Root, Not Just the Symptoms
One of Dr. Lu’s most compelling findings is that sleep therapy can improve mental health even when total sleep hours don’t change significantly. In one study, participants with traumatic brain injuries completed just four CBT-I sessions. The results? Better sleep quality, improved mood, and reduced anxiety.
This suggests that how we sleep may matter just as much as how much we sleep—and that sleep could be a foundational pillar in treating complex conditions like PTSD, depression, and anxiety.
Ready to Sleep and Heal Better?
Can sleep heal more than we think? If you’ve tried everything else—medication, melatonin, white noise, but still can’t sleep, CBT-I may be the solution. At Dr. Iospa Psychiatry, we’re here to help you restore not just sleep, but clarity, energy, and emotional peace.
Reclaim Your Rest?
Dr. Iospa Psychiatry Consulting offers in-person and telehealth services throughout New York City, including Manhattan, Queens, Brooklyn, and Long Island. If you or someone you love is struggling with sleep, depression, anxiety, or PTSD, reach out to schedule an evaluation with one of our clinicians.
Contact us today to learn more about CBT-I and how sleep can become an integral part of your healing proce